Why Antibiotics Won’t Fix Your Cough or Congestion! Other Options Can Help You Breathe Easier.
When a cough lingers for days, your sinuses feel blocked, or your throat is scratchy and raw, it’s completely normal to want fast relief. Many people assume the quickest way to feel better is to get an antibiotic prescription. After all, antibiotics have been around for decades, and we’re used to receiving them “just in case” when we’re not feeling well. But the truth is that most respiratory symptoms—especially semi-productive coughs, congestion, sinus pressure, and sore throats—are caused by viral infections, not bacterial ones. This means antibiotics won’t help, and in many cases, taking them can actually create new problems.
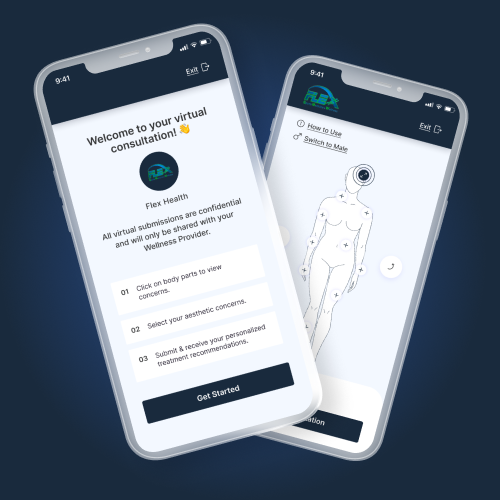
Understanding the difference between viral and bacterial infections, and knowing what treatments truly work, can help you recover faster and avoid unnecessary medications. At Flex Health, we want you to feel better quickly while also receiving the safest, most effective care. This guide breaks down why antibiotics often aren’t needed and what you should reach for instead.
Most Coughs and Congestion Are Caused by Viruses, Not Bacteria
The majority of respiratory illnesses we see—whether in kids, teens, or adults—are caused by viruses. These include the common cold, viral bronchitis, influenza, RSV, COVID-19, and other seasonal viruses. Although each of these infections can feel different, they tend to cause a similar cluster of symptoms: a semi-productive or phlegmy cough, nasal congestion, post-nasal drip, sinus pressure, sore throat, mild fatigue, and sometimes a low-grade fever.
Many patients are surprised to learn that these symptoms don’t necessarily indicate a bacterial infection. For example, the color of mucus—yellow, green, cloudy, or thick—does not tell us whether you need antibiotics. This misconception has been passed down for years, but medically, it has no reliable significance. Viral infections commonly cause changes in mucus color due to inflammatory cells, not bacteria.
Another common belief is that if a cough lasts more than a few days, it must require antibiotics. In reality, viral coughs can last anywhere from 1 to 4 weeks, depending on the virus and your immune system’s response. Post-viral coughs—often caused by lingering airway inflammation—can take even longer to resolve.
Understanding that most respiratory illnesses are viral is the first and most important step in choosing the right treatment.
Why Antibiotics Don’t Help Viral Respiratory Illnesses
Although antibiotics are incredibly valuable for true bacterial infections, they have no effect on viruses. They don’t reduce the severity of
symptoms, shorten the duration of illness, or prevent the virus from spreading. But unnecessary antibiotics don’t just fail to help—they come with real downsides.
1. Antibiotics don’t shorten recovery time.
Viral respiratory illnesses simply need time to run their course. Your immune system is what clears the virus, not medication. Antibiotics won’t soothe your throat, open your sinuses, or relieve your cough. They won’t help you get back to work faster, and they won’t prevent complications.
2. Antibiotics can cause avoidable side effects.
Even when taken for the right reason, antibiotics can cause:
-
Nausea
-
Diarrhea
-
Abdominal cramping
-
Yeast infections
-
Medication interactions
-
Allergic reactions
When antibiotics are not needed, these side effects are both unnecessary and avoidable.
3. Antibiotics disrupt your gut microbiome.
Antibiotics don’t only target harmful bacteria—they also wipe out beneficial bacteria in the gut. This imbalance can affect digestion, immune function, and even mood. Restoring the microbiome can take months.
4. Overuse contributes to antibiotic resistance.
One of the biggest long-term risks of unnecessary antibiotics is resistance. When bacteria are repeatedly exposed to antibiotics, they adapt and become harder to treat. Resistant infections can become dangerous, expensive, and difficult to manage—and they affect communities, not just individuals.
Choosing not to take antibiotics for viral illnesses isn’t just good for you—it’s good for public health.
What Does Help: Effective, Evidence-Based Relief
Even though antibiotics don’t treat viral respiratory infections, there are many therapies that can significantly improve your comfort and help you breathe easier. These interventions target inflammation, drainage, congestion, and irritation—the real drivers of your symptoms.
1. Nasal steroid sprays (fluticasone, triamcinolone, mometasone)
Nasal steroid sprays are among the most effective treatments for congestion, sinus pressure, and post-nasal drip. They work by reducing inflammation inside the nose and sinus passages, making it easier to breathe and reducing the mucus that drips down the back of your throat and triggers coughing.
Unlike nasal decongestant sprays (like Afrin), steroid sprays are safe for daily use and do not cause rebound congestion. However, they work best when used consistently—usually taking 24–72 hours to reach full effect.
They help:
-
Open sinus passages
-
Reduce swelling and pressure
-
Improve drainage
-
Decrease cough caused by mucus
Many patients feel significantly better within a few days simply by using a nasal steroid spray correctly and consistently.
2. Pseudoephedrine (Sudafed): The “real” oral decongestant
Pseudoephedrine is highly effective at relieving sinus pressure and nasal congestion. It works by constricting swollen blood vessels inside the nasal passages, allowing air to pass through more freely. It can be especially useful during the day when congestion interferes with breathing, productivity, or daily activities.
Pseudoephedrine can help:
-
Ease sinus pressure
-
Reduce facial fullness
-
Improve airflow
-
Decrease ear pressure
-
Support drainage
It’s important to note that pseudoephedrine is different from phenylephrine—the ingredient found in many “non-drowsy” cold medications, which research shows is often ineffective. This is why pseudoephedrine is kept behind the pharmacy counter.
Patients with hypertension, glaucoma, or certain heart conditions should consult a clinician before using pseudoephedrine. For most people, however, it is a very helpful and appropriate choice.
3. Hydration and humidity
Hydration is one of the simplest but most powerful tools for viral illness recovery. Fluids thin mucus secretions, lubricate the throat, and support immune function. Warm liquids, such as tea with honey, broths, and herbal infusions, soothe throat irritation and help break up congestion.
Humidity also plays a major role. Using a humidifier or inhaling steam can loosen mucus and relieve airway irritation, making breathing more comfortable and coughing less intense.
4. Over-the-counter symptom support
Several OTC options can help relieve symptoms while your body clears the virus:
-
Guaifenesin (Mucinex) helps thin mucus, making coughs more productive and reducing chest congestion.
-
Saline nasal rinses flush out mucus, allergens, and irritants.
-
Acetaminophen or ibuprofen relieve fever, aches, and throat pain.
-
Honey is a proven nighttime cough suppressant (for adults and children over 1 year).
These treatments don’t cure the infection, but they support your body and make recovery significantly more comfortable.
5. Rest and recovery
Your immune system functions best when you are resting. Continuing to push through fatigue can prolong symptoms and weaken your body’s ability to fight infection. Giving yourself permission to slow down—emotionally and physically—is often a key part of healing.
When Antibiotics Are Appropriate
Although unnecessary in most cases, antibiotics are sometimes essential. Recognizing the difference between viral and bacterial infections is crucial. Seek medical evaluation if you experience:
-
Fever over 101.5°F lasting more than 48–72 hours
-
Severe sinus pain lasting over a week
-
Symptoms that worsen after initial improvement
-
Classic strep throat symptoms (severe throat pain, fever, swollen lymph nodes, and no cough)
-
Shortness of breath, chest pain, or signs of pneumonia
-
A cough lasting longer than 3–4 weeks
In these cases, your clinician may perform a rapid strep test, throat culture, chest exam, viral swab, or imaging to determine whether antibiotics are warranted. At Flex Health, we focus on accuracy—not guesswork—to ensure you get the right treatment.
The Bottom Line
Most cases of cough, congestion, and sore throat are caused by viruses—not bacteria—meaning antibiotics won’t help and may even cause harm. Instead, tools like nasal steroid sprays, pseudoephedrine, hydration, humidity, and rest can provide meaningful relief while your body heals naturally.
If you’re unsure whether your symptoms require antibiotics, or you simply want guidance on what helps you feel better fastest, Flex Health is here to help. We focus on personalized, evidence-based care that prioritizes your safety, comfort, and long-term health.