Women’s Hormones: Myths, Facts, and Evidence-Based Treatments
Hormones influence nearly every aspect of a woman’s health — from mood and metabolism to sleep, fertility, and cognitive function. Yet despite their importance, women’s hormones are often surrounded by confusion and misinformation. Hormonal changes are a natural part of life, but misunderstanding them can lead to unnecessary fear or ineffective treatments. Understanding what’s true, what’s myth, and what modern medicine can offer is the foundation of informed, confident care.
Hormonal Changes Occur Throughout Life
A common misconception is that hormonal changes only matter during menopause. In reality, hormone fluctuations begin much earlier and continue throughout a woman’s life. Puberty, menstruation, pregnancy, postpartum recovery, and perimenopause all bring hormonal shifts that can affect mood, sleep, and physical health.
Perimenopause, the gradual transition before menopause, can start earlier than many realize — sometimes as early as a woman’s mid to late 30s. During this time, estrogen and progesterone levels fluctuate unpredictably, leading to symptoms such as irregular cycles, night sweats, anxiety, and changes in libido or concentration. Recognizing early perimenopause helps women seek evaluation and support before symptoms intensify or quality of life declines.
Hormones Are Not Always to Blame for Fatigue or Mood Changes
Feeling tired, irritable, or moody doesn’t always mean hormones are “out of balance.” These symptoms can also stem from stress, poor nutrition, lack of sleep, or thyroid and adrenal dysfunction. Because multiple systems interact with one another, a comprehensive evaluation is essential. Laboratory testing—paired with a discussion of lifestyle, diet, and mental health—helps determine whether hormones truly play a role or whether other factors need attention first.
Self-diagnosing or chasing the latest “hormone-balancing” trend can often overlook underlying causes and delay effective care.
Modern Hormone Therapy Is Safer Than Many Think
Hormone replacement therapy (HRT) once carried a reputation for risk, largely due to outdated research using synthetic hormones. Today, studies show that bioidentical and FDA-approved hormone therapies, when prescribed thoughtfully and monitored closely, are safe and effective for most women.
For many, HRT provides significant relief from hot flashes, sleep disturbances, mood changes, and vaginal dryness while also supporting bone and heart health. However, like any medical treatment, HRT must be individualized. The type of hormone, dose, and delivery method should all be carefully chosen based on a woman’s health history and risk profile.
Understanding Testosterone Therapy and Pellet Risks
Testosterone isn’t just a male hormone — women produce it naturally, too. It plays a key role in energy, libido, muscle tone, and mental focus. When testosterone levels are low, some women may benefit from carefully dosed replacement therapy. However, it’s important to understand that not all delivery methods are equally safe.
One option that has gained popularity is the use of testosterone pellets, which are implanted under the skin and release hormones over several months. While convenient, pellets can lead to unpredictable hormone levels, sometimes producing excessive testosterone exposure. This may cause acne, hair growth, mood changes, or even irreversible voice deepening. Because the pellets cannot be easily adjusted or removed once inserted, they carry a higher risk of overtreatment compared to topical or oral methods. These have even been mentioned in a link to certain female cancers.
Medical experts generally recommend starting with short-acting, adjustable formulations to ensure hormone levels remain within a safe and physiologic range.
Supplements Alone Cannot “Balance” Hormones
Another myth is that vitamins or herbal products can fully balance hormones on their own. While certain nutrients support healthy hormone metabolism and stress regulation, supplements cannot directly replace estrogen, progesterone, or testosterone. The best approach combines nutritional support, physical activity, adequate sleep, and, when indicated, medically guided hormone therapy. True hormonal balance comes from addressing the whole body—not just taking a pill or powder.
Menopause Is a New Chapter, Not the End of Vitality
Menopause often carries a negative reputation, but it is not a loss of femininity or vitality. It’s simply a natural phase in a woman’s life when the ovaries produce less estrogen and progesterone. With proper care—including nutrition, exercise, and, for some, hormone therapy—women can maintain energy, cognitive sharpness, and sexual health well into their later years. Menopause is a transition, not an ending.
How Hormones Work Together
The body’s hormonal network functions in balance. Estrogen supports reproductive health, bone density, and brain function. Progesterone promotes restful sleep, mood stability, and uterine health. Testosterone enhances libido and motivation. Thyroid hormones drive metabolism and energy, while cortisol manages the stress response. Insulin controls blood sugar, and imbalances can disrupt reproductive hormones. When one hormone shifts, others adjust in response, underscoring the importance of comprehensive testing and holistic treatment.
When Hormone Testing Is—and Isn’t—Helpful
Many women wonder whether checking their estrogen and progesterone levels can explain symptoms such as fatigue, hot flashes, or mood changes. In most cases, however, routine blood testing for these hormones offers limited clinical value—especially in women who are still having menstrual cycles.
Estrogen and progesterone levels naturally fluctuate throughout the month, sometimes dramatically from day to day. A single blood test provides only a snapshot in time and doesn’t necessarily reflect overall hormonal health or explain ongoing symptoms. For example, estrogen may be high one week and low the next, even in perfectly normal cycles. Because of this variability, test results can be misleading or easily misinterpreted.
Instead of relying heavily on these lab numbers, clinicians often focus on a woman’s symptoms, age, menstrual history, and overall health to guide evaluation and treatment. For perimenopausal and menopausal women, the diagnosis is typically clinical, based on changes in cycle regularity and symptoms rather than on specific hormone values.
That said, hormone testing can still play a role in some situations—such as assessing thyroid function, cortisol patterns, or testosterone levels when appropriate. These hormones are more stable and often provide clearer diagnostic insight.
In short, while testing can be a useful tool in select cases, it’s important to interpret results within the broader context of the patient’s experience, rather than treating lab values in isolation.
Evidence-Based Treatments for Hormonal Health
Achieving hormonal balance starts with lifestyle. A nutrient-dense diet rich in fiber, healthy fats, and plant-based phytoestrogens (such as flaxseed and soy) supports natural hormone production. Regular strength training, walking, and adequate sleep improve metabolism and resilience. Managing stress through mindfulness, yoga, or breathing exercises helps regulate cortisol and improve overall well-being.
When symptoms persist, testing can provide clarity. Blood or saliva panels may assess levels of estrogen, progesterone, testosterone, thyroid hormones, and cortisol. Based on the results, clinicians can tailor treatment using bioidentical hormone replacement therapy (HRT) in safe, adjustable forms like creams, patches, or oral capsules.
Supportive therapies—such as vitamin D, magnesium, and omega-3s—enhance cellular health and hormone metabolism. The ultimate goal is not to chase “perfect” lab numbers but to restore balance and improve quality of life.
The Benefits of Balanced Hormones
When hormones are properly managed, women often experience improved mood, better sleep, higher energy, and enhanced cognitive clarity. Libido and muscle tone may increase, while skin and hair health often improve. Beyond symptom relief, maintaining hormonal balance supports long-term wellness, bone strength, and heart health.
Conclusion
Women’s hormones are complex, but they don’t have to be mysterious. Myths about perimenopause, testosterone therapy, or “hormone balancing” supplements can create confusion or delay care. In truth, hormonal changes are a normal and expected part of life. With accurate information, appropriate testing, and individualized treatment, women can navigate these transitions with clarity and confidence. Hormonal health isn’t about reversing time—it’s about living vibrantly through every stage of life.
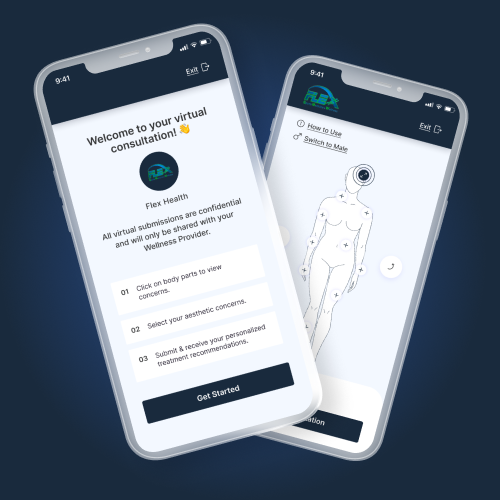
For more information, schedule your appointment to learn about treatment options for women’s hormones in Evans, GA at Flex Health.